Final practicals -Exam Cases
47 year old male patient who worked in steel company, currently disabled because of his health issues presented to us with history of
Cheif complaints :
1-Tingling and Numbness of both lower limbs since 5 years .
2- ulcer over left foot since 4 months
3-one episode of Involuntary movements of upper and lower limb 10 days back.
History of presenting illness :
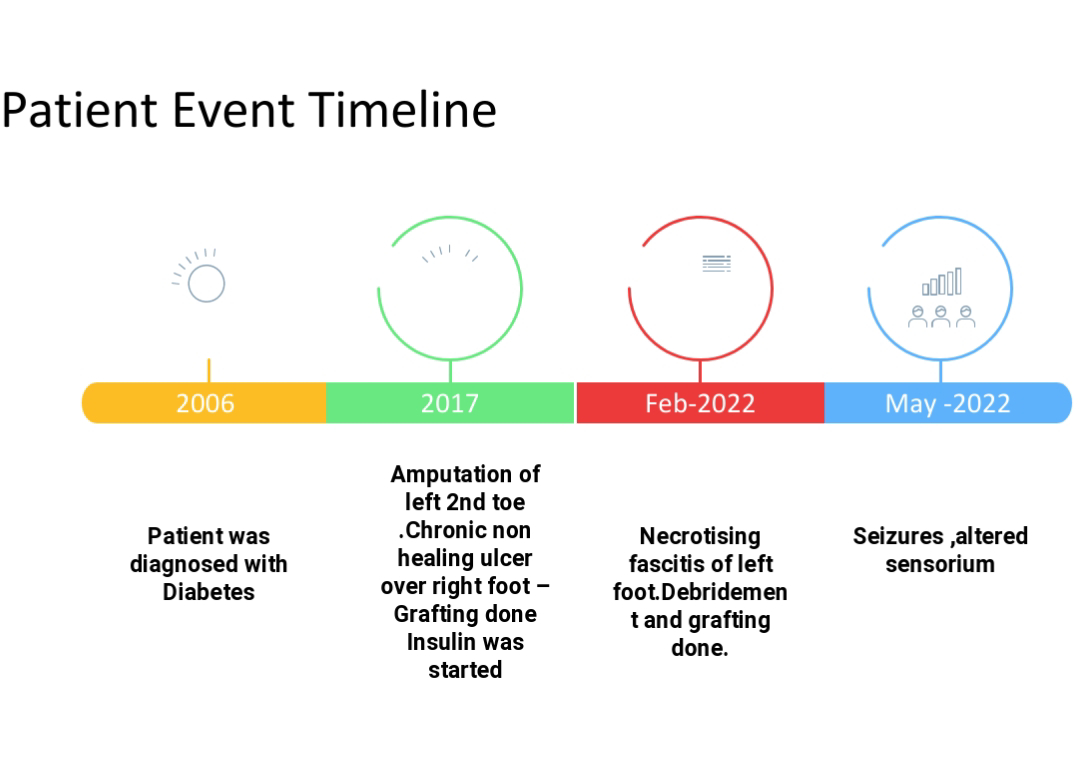
His history dates back to 15 years when he visited hospital for the fever and on investigations he was found to be diabetic .He used oral hypoglycemia agents initially for 5 years and was on followup.He was complaint to medications and had no health issues.
Later he developed tingling and Numbness of both foot since 5 years ,which he ignored initially as the symptoms were intermittent and not disabling .
Then he noticed redness and swelling of left lower limb ,that progressed to blisters and ulcer over dorsal aspect of left foot.
After few days there was discoloration of left 2nd toe for which he was hospitalized and his left 2 nd toe was amputated .But the ulcer progressed to forefoot,so regular dressings were done and skin grafting was done .During this hospitalisation he was advised to use insulin for daibetes.He was prescribed Insulin Human Mixtard 18 u in the morning and 12 units in the night before food.
His ulcer resolved over 3 months .
Since 4 years patient complaints of loss of sensation over both foot till ankle .It was gradual in onset and progressed to current state. He was unable to perceive hot or sensation in both lower limbs till ankle region .He couldn't perceive the pain sensation following an injury .He also complaints of cotton wool sensations .
There were episodes of frequent slippage of footwear unknowingly .
Since 1 year he is complaining of tingling and numbness over fingertips intermittently.
There were washbasin attacks.No history of swaying or gait disturbances.
No difficulty in getting up from sitting or squatting position.
No difficulty in climbing stairs
No difficulty in combing hair , buttoning and unbuttoning shirt ,mixing food.
No history of falls
No bowel and bladder disturbances.
No abnormal sweating and no postural instability or syncopal attacks .
Inspite of all these symptoms he never consulted a doctor .
Then after 4 months back , patient noticed small ulcer on the same foot for which he was grafted previously .Within no time ulcer progressed and he got admitted in our hospital . Daily dressings were done and was advised for grafting .
Patient went home and on returning back to the hospital on motor bike, patient suffered burn injury to right foot by the silencer .He couldn't perceive the pain , throughout the journey ,he noticed it after he reached the hospital ,which was taken care after admission.
On 13/5/2022 grafting was done ,and he was kept under observation ,his post operative events were uneventful, hence shifted to general ward .On 23/5/2022 patient had suddenly developed involuntary movements of both upper and lower limbs for 1 minute associated with loss of awareness, drooling of saliva ,uprolling of eye balls ,and involuntary defecation .
No head injury ,tongue bite.
Following this patient was drowsy for the next 2 days ,with intermittent regaining of consciousness.
No history of similiar complaints in the past.
No history of fever , headache , vomitings.
No speech dustubances ,no difficulty in swallowing ,no visual dustubances ,no weakness of limbs ,no sensory disturbances .
Past history :
He is Diabetic since 15 years and on insulin therapy since 10 years.
Hypothyroidism since 1 month .
No history of coronary artery disease ,renal failure, cerebrovascular accident.
No significant family history .
Personal history :
Patient has normal appetite .
He is an Occasional alcoholic
Tobacco chewer since 10 years - 2 packets / day.
No high risk behaviour.
No bowel and bladder disturbances
Provisional diagnosis :
1-Bilateral distal Symmetric peripheral neuropathy secondary to ?diabetes.
2- Chronic non healing, recurrent ulcers secondary to ? diabetic microvascular complications
3- Generalised tonic clonic seizures - secondary to
?Hypoglycemia
?Acute Ischemic or hemorrhagic CVA
?Electrolyte disturbances
On examination :
General examination :
Patient is thin built ,with loss of buccal pad of fat ,and temporal muscle wasting .
No pallor ,icterus ,cyanosis ,clubbing ,lymphadenopathy ,edema .
Ulcer on right and left foot.
No peripheral nerve thickening.
No hypo pigmented patches .
Vitals :
Patient is afebrile to touch.
Radial Pulse - 90 beats per minute , regular, normal volume ,normal character.
Popilteal artery - feeble pulse felt on both sides.
Dorsalis pedis artery and tibialis anterior couldn't be appreciated.
No radio radial delay ,no radiofemoral delay .
BP - 110/80 mmhg ,meaured in supine position ,in both arms .
Lower limbs BP -100/80 mmhg on both sides.
RR -16 breaths / min
Systemic examination :
Higher mental functions :
Patient is conscious, coherent co-operative .
Memory ,language ,recall ,naming ,comprehension ,calculation are intact.
Cranial nerves :
Motor system examination :
Reflexes :
Sensory system examination :
Cerebellar signs :
No intention tremors
No rebound phenomenon
No nystagmus
No finger finger or finger nose incordination
No pastpointing
Examination of spine - Normal .
Examination of other systems :
Respiratory system :
Trachea central in position.
Bilaterally symmetrical chest and no abnormalities.
Auscultation - normal vesicular breath sounds heard in all lung feilds .
Cardiovascular system :
No raised JVP
Apex impulse 5th intercostal space 1 cm medial to midclavicular line.
S1 and S2 heard
No murmurs .
Gastrointestinal system :
Abdomen is scaphoid .
Soft and non tender .
No organomegaly.
Impression :
Distal Symmetric sensory - length dependent peripheral neuropathy( axonal variant ) .
Small and large fibre neuropathy.
Approach to patient :
1- Seizures - After initial stabilisation of the patient ,a metabolic panel was ordered and patient was found to be having severe hyponatremia of Serum sodium -117 , Immediate slow sodium correction was started .
His corrected sodium was - 120 meq for GRBS value of 290 mg/dl.
( Pseudohyponatremia was excluded )
His serum osmolality was 264 mosm.
Urine dipstick showed - urine sugars 4+
Patient was neither in overload state nor in severe dehydration on examination.
In view of euvolemic hyposmolar hyponatremia he was further investigated to identify the cause of hyponatremia .
Urine osmolality was not available ,so it was not sent .
with clinical examination and available investigations two possible differentials were thought as cause for the hyponatremia,after excluding drugs,CNS and other causes.
1- Hypothyroidism
2- SIADH
Cause of hyponatremia in our patient appears to be multifactorial :
a) chronic hospitalisation
b) poor nutrition
c) Diabetes - osmotic diuresis
d) infusion of isotonic salines that stimulate ADH and cause hyponatremia.
e) surgery .
2 Diabetic Complications:
In view of long standing Diabetes screening for target organ damage was done with history,examination and necessary investigations.
Clinical examination mentioned above is suggestive of Distal Symmetric peripheral neuropathy,Fundus showed retinopathy changes .
CUE - 4+ albumin ,4+ sugars
Spot urine Protein creatinine ratio revealed proteinuria.
Arterial Doppler of both lower limbs :
Other investigations :
2D echo :
Serology negative .
Serum creatinine -1.2 mg/dl .
Blood urea - 42mg/dl.
Serum calcium-10.2 mg/dl.
Final Diagnosis:
1.Seizures secondary to hyponatremia
2.Chronic progressive Distal symmetric sensory predominant ,peripheral neuropathy
Length dependent pattern .
Small and large fibre Neuropathy .
secondary to Diabetes.
3.Necrotising Fascitis of left foot s/p of grafting,in the phase of healing .
4- Diffuse atherosclerosis of lower limb vessels - Peripheral artery disease .
5.Diabetic nephropathy ,Non proliferative Diabetic retinopathy.
Discussion :
How do we screen and manage diabetes patient with Neuropathy symptoms ? :
Early detection and management .
The American Diabetes Association
recommends that patients with type 1 diabetes for ≥5 years and all patients with type 2 diabetes should be assessed for DSPN annually, including a medical history to assess for symptoms and a combination of at least two of the examinations :
Tests for small-fiber function: pinprick (push pin) and temperature sensation (1)
Tests for large-fiber function: vibration perception with a 128-Hz tuning fork, proprioception.
Rehabilitation :
Lifestyle modification .
Diabetic foot management.
Exercise training.
------------------------------------------
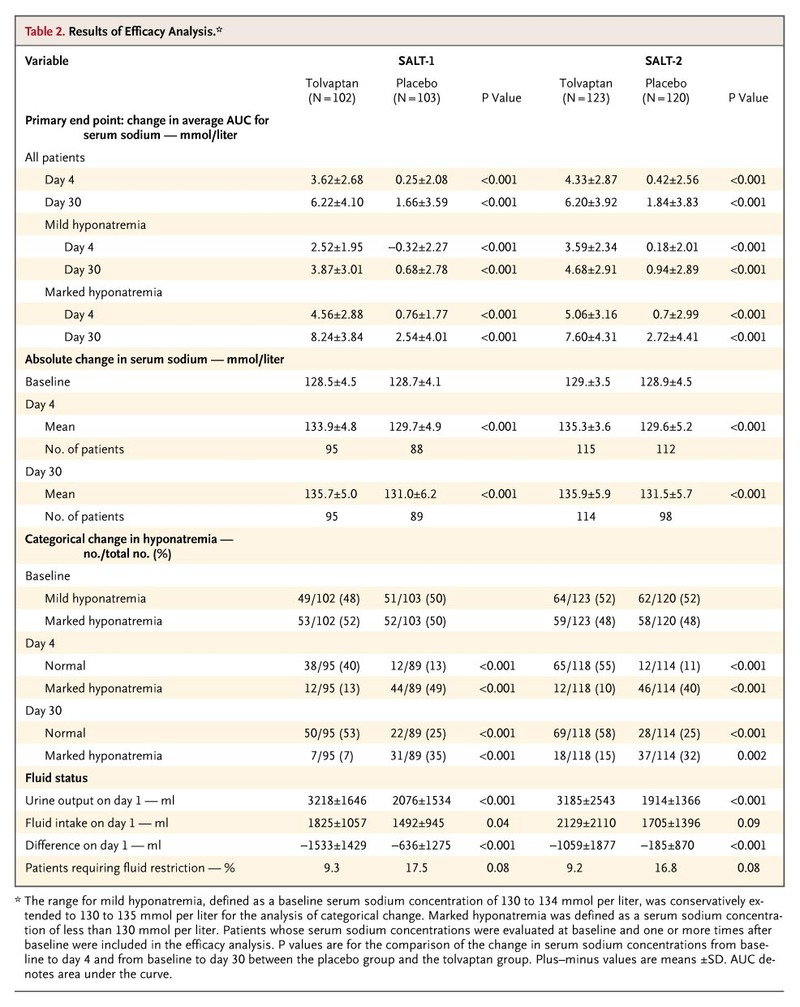
Efficacy of Tolvaptan in hyponatremia - SALT 1 & SALT 2 trials.
https://www.nejm.org/doi/full/10.1056/nejmoa065181
In two multicenter, randomized, double-blind, placebo-controlled trials, the efficacy of tolvaptan was evaluated in patients with euvolemic or hypervolemic hyponatremia.
P- patient with evolemic or hypervolemic hyponatremia.
I- Tolvaptan 15 mg -30/60 mg
C- compared to placebo
O-- In patients with euvolemic or hypervolemic hyponatremia, tolvaptan, an oral vasopressin V2-receptor antagonist, was effective in increasing serum sodium concentrations at day 4 and day 30..
Patient characteristics :
--------------------------------------------------------------------------------------------
Short case 1 :
51 year old male patient who is resident of Suryapet ,and works in Good transportation company came to the hospital with complaints of
1- Fever since 10 days
2- Cough since 10 days
3-shortness of breath since 6 days
History of presenting illness :
Fever since 10 days which is high grade , with chills and rigors , intermittent ,relieving with medication.
Associated with cough and shortness of breath.
Cough since 10 days which is productive ,mucoid in consistency,whitish ,scanty amount ,more during night times and on supine position ,non foulsmelling ,non bloodstained .
Right sided chest pain - diffuse , intermittent ,dragging type , aggravated on cough ,non radiating ,not associated with sweating , palpitations.
Shortness of breath since 6 days , insidious onset , gradually progresive ,of grade 3 - (MMRC scale ),not associated with wheeze ,no orthopnea ,no Paroxysmal nocturnal dyspnea, no pedal edema .
No history of weight loss ,no loss of appetite
No history of pain abdomen or abdominal distension , vomitings ,loose stools .
No history of burning micturition.
Past history :
Patient gives history jaundice 15 days back that resolved in a week .
No history of Diabetes , Hypertension , Tuberculosis ,Bronchial asthma ,COPD , coronary artery disease , Cerebrovascular accident ,thyroid disease.
Family history :
No history of Tuberculosis or similar illness in the family
Personal history :
Patient is a chronic smoker - smokes 5 cigarettes per day from past 25 years .
He is a Chronic alcoholic - cosumes 300 ml whisky per day ,but stopped since 3 months.
No bowel and bladder disturbances
Summary :
51 year old male patient with fever ,cough , shortness of breath possible differentials
1- Pneumonia
2- Pleural effusion
GENERAL EXAMINATION :
Patient is moderately built and nourished.
He is conscious, comfortable.
No signs of pallor ,cyanosis ,icterus ,koilonychia , lymphadenopathy ,edema .
Vitals :
Patient is afebrile .
Pulse - 86 beats / min ,normal voulme ,regular rhythm,normal character ,no radiofemoral delay.
BP - 110/70 mmhg ,measured in supine position in both arms .
Respiratory rate -22 breaths / min
SYSTEMIC EXAMINATION :
Patient examined in sitting position
Inspection:-
Upper respiratory tract - oral cavity- Nicotine staining seen on teeth and gums , nose & oropharynx appears normal.
Chest appears Bilaterally symmetrical & elliptical in shape
Respiratory movements appear to be decreased on right side and it's Abdominothoracic type.
Trachea is central in position & Nipples are in 4th Intercoastal space
Apex impulse visible in 5th intercostal space
No signs of volume loss
No dilated veins, scars, sinuses, visible pulsations.
No rib crowding ,no accessory muscle usage.
Palpation:-
All inspiratory findings are confirmed
Trachea central in position
Apical impulse in left 5th ICS, 1cm medial to mid clavicular line
Cricosternal distance is 3finger breadths.
Other systems examination :
Gastrointestinal system :
Inspection -
Abdomen is distended.
Umbilicus is central in position.
All quadrants of abdomen are equally moving with respiration except Right upper quadrant .
No visibe sinuses ,scars , visible pulsations or visible peristalsis
Palpation:
All inspectory findings are confirmed.
No tenderness .
Liver - is palpable 4 cm below the costal margin and moving with respiration.
Spleen : not palpable.
Kidneys - bimanually palpable.
Percussion - normal
Traubes space
Auscultation- bowel sounds heard .
No bruits .
Cardiovascular system -
S1 and S 2 heard in all areas ,no murmurs
Central nervous system - Normal
Final Diagnosis :
1- Right sided Pleural effusion likely infectious etiology.
2- Hepatomegaly - ? Hepatitis or ? Chronic liver disease
Investigations :
Pleural fluid analysis :
Colour - straw coloured
Total count -2250 cells
Differential count -60% Lymphocyte ,40% Neutrophils
No malignant cells.
Pleural fluid sugar = 128 mg/dl
Pleural fluid protein / serum protein= 5.1/7 = 0.7
Pleural fluid LDH / serum LDH = 190/240= 0.6
Interpretation: Exudative pleural effusion.
Other investigations :
Serology negative
Serum creatinine-0.8 mg/dl
CUE - normal
CT abdomen :
Final Diagnosis:
1-Right sided Pleural effusion - synpneumonic effusion
2- Liver Abscess .
_______________________________________________________
Short case 2:
62 year old female patient who is a housewife came to the hospital with chief complaints of
1.shortness of breath since 7 years .
2.bilateral pedal edema since 7 years .
History of presenting illness :
Patient was apparently assymptomatic 7 years back then she developed left sided chest pain associated with shortness of breath .She was hospitalized and angiography was done which showed CORONARY ARTERY DISEASE-double vessel wall disease and PTCA to RCA was done in 2015 ,since then patient complaints of intermittent shortness of breath with intermittent exacerbations of symptoms.
Her symptoms aggravated 2 years back and she was admitted in our hospital for 1 week.
patient finds difficulty even for walking short distance like walking to the bathroom and has to stop in between due to breathlessness .
She also complaints breathless while climbing stairs .
Patient gives history of PND and orthopnea .
She never complained of chest pain , palpitations , syncopal attacks , giddiness ,chest tightness ,cough , wheeze .
She gives history of Swelling of both lower limbs till knee since 7 years ,that slightly reduces after recumbency .
There is no frothing of urine , decreased urine output , hematuria .
No history of jaundice ,pain abdomen , abdominal distension.
Past history :
Patient is k/c/o T2 DM since 7 years on glycomet M2 once daily
K/c/o HTN since 7 years on Telmisartan 80 mg /once daily
K/c/o CAD- on clopidogrel 75 mg /once daily ,Atorvastatin 20 mg / hs.
History of 2 PRBC transfusions done
GENERAL EXAMINATION :
Patient is well built and obese.
Pallor ++
Dyspnea +
Pedal edema - grade 2 ,bilateral , pitting
Raised Jugular venous pressure
Pulse rate - normal volume ,regular in rhythm ,94 beats / min ,normal character,no radiofemoral,no radioradial delay,all peripheral pulses were felt .
BP- 150/100 mmhg in both arms
No signs of invective endocarditis, congenital or valvular heart diseases.
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM -
Inspection :
Chest is bilaterally symmetrical
No precordial bulge
Apex impulse visible in 5th intercostal space
No parasternal ,supraclavicular,epigastric pulsations .
No visible sinus ,scars ,dilated veins.
s1 and s2 heard ,no murmurs
Palpation :
All inspectory findings are confirmed
Apex impulse - felt in 5th intercostal space ,1 cm medial to midclavicular line
No parasternal heave ,no palpable thrills .
Auscultation :
Mitral area - S1 and S2 heard ,no murmurs
Aortic area - S1 and S2 heard ,no murmurs
Pulmonary area - S1 and S2 heard ,no murmurs
Tricuspid area - S1 and S2 heard ,no murmurs
Other systems :
Respiratory system : normal vesicular breath sounds heard in all lung fields .
Per Abdomen -soft ,non tender
CNS- normal
Provisional diagnosis:
1.Shortness of breath secondary to ? Chronic Heart failure
2. Anemia
3. Known case of Diabetes , Hypertension and Coronary artery disease .
Investigations :
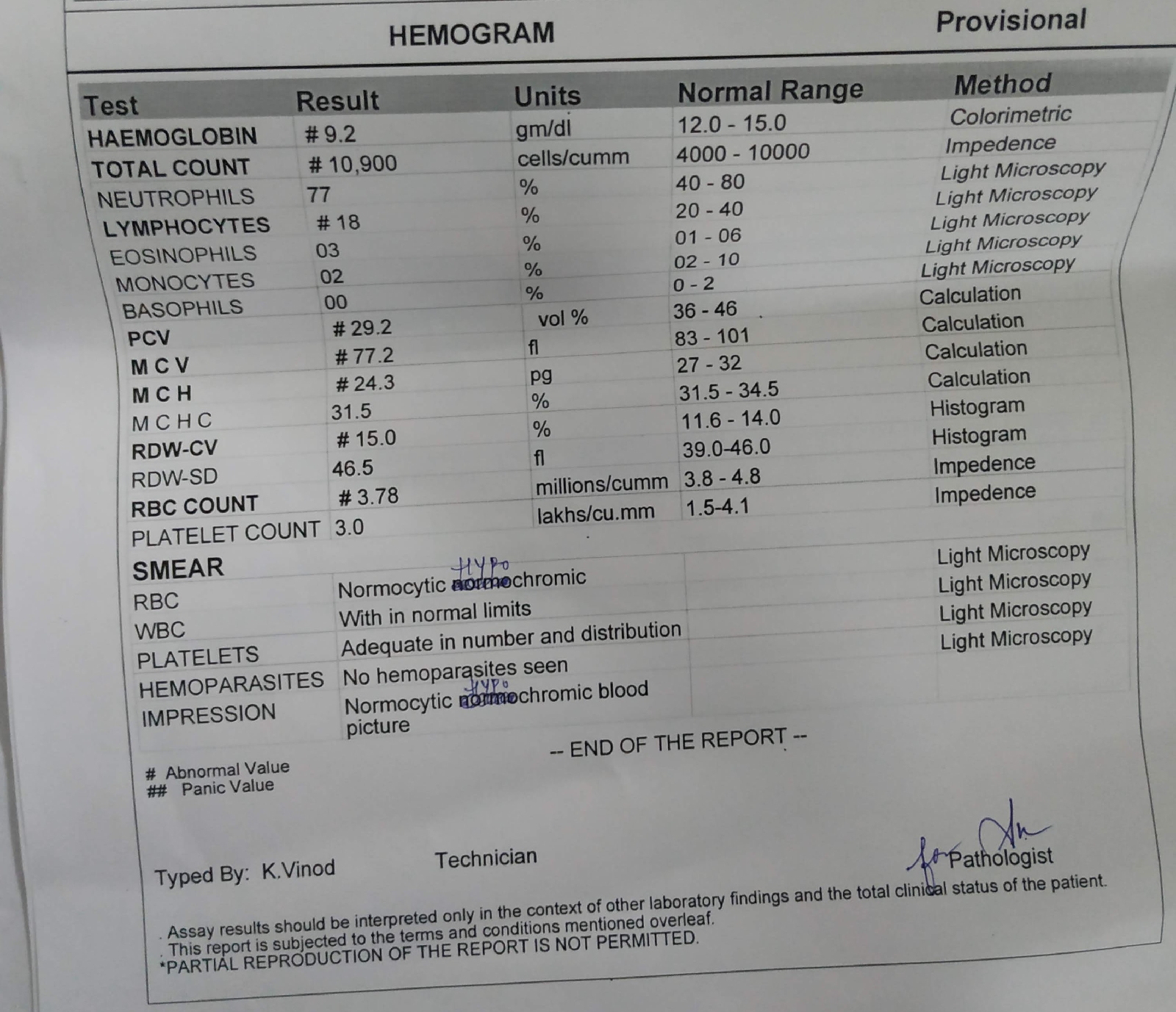
Complete blood picture showed Normocytic hypochromic anemia
Cue - normal
LFT -
Ecg -
2D ECHO showed :
Concentric Left Ventricular hypertrophy
With ejection fraction near -58% .
All other chambers are normal.
No valvular regurgitant or stenotic lesions.
No pericardial effusion.
Final Diagnosis:
1.Chronic Heart failure - Heart failure with preserved ejection fraction.
2.known case of Diabetes ,Hypertension , Coronary artery disease.













































Comments
Post a Comment