January exam
This is my submission to online exam of January month .
1- 26 year old woman with complaints of altered sensorium since 1 day,headache since 8 days,fever and vomitings since 4 days
More here: https://harikachindam7.blogspot.com/2020/12/26-year-old-female-with-complaints-of.html
A) What is the problem representation of this patient and what is the anatomical localization for her current problem based on the clinical findings?
Problem representation :
1- 26 year old female patient with multiple small joint pains since 6 years - on immunosuppressive treatment.
2- Gradually progressive headache since 1 month
3-Exposure to tuberculosis .
4-Acute onset of vomitings ,fever and altered sensorium since 1 week .
Anatomical Localisation of current problem - (fever , headache , vomitings,altered mental status )
1- Raised Intracranial pressure
2- Acute febrile illness- Viral / bacterial - Anatomical localisation - CNS
3-Electrolyte abnormalities secondary to vomitings - hyponatremia
4- CNS - lupus
5- steriod withdrawal causing hyponatremia
6- Patient was found on floor with altered sensorium - history of fall ? Head trauma ? Causing altered sensorium ?
B) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of her problems and current outcomes
Sequence of events -
1)Multiple joint pains - diagnosed with SLE on treatment.
2)Headache since 1 month , gradually progressive
3)History of fever ,vomitings for 4 days followed by acute onset of altered sensorium
Possible differential diagnosis include :
1- Infection - Meningitis , encephalitis
2- inflammation - CNS lupus
3- Traumatic
4- neoplastic
5-CVA
6- Toxin
As patient presented to us in altered sensorium , irrelevant talk,we took detailed history and examined her .
GCS was - E3V3M5
We checked pupillary response to light - it was equal and responsive to light .
Neck rigidity was absent
Brudzinkis and kernigs negative
Respiration was normal
Vitals were stable
With the history provided by the attenders we thought of following possible diagnosis
1- Hyponatremia secondary to vomitings
2- Meningitis/ Encephalitis
3- CVA - ischemic / hemorrhagic
We have sent metabolic profile and urine electrolytes and serum osmolality .
Once we confirmed that she is having hyponatremia - we started treating her as Acute symptomatic hyponatremia - with 3% Nacl .
So we have put our provisional daignosis as euvolemic hyponatremia- SIADH .
( patient appeared to be well hydrated as she was treated in outside hospital with fluids and other supportive Treatment).
We got MRI on next day
And did CSF analysis - It turned out to be CBNAAT positive .
As there is significant exposure to tuberculosis and also CBNAAT +
With clinical history of chronic Headache ,on immunosuppression
She was started on ATT .
c) What is the efficacy of each of the drugs listed in her prior treatment plan that she was following since last two years before she stopped it two weeks back?
Efficacy of Hydroxychloroquine in sle
https://pubmed.ncbi.nlm.nih.gov/31777844/
This study is retrospective , focused on outcomes of patients who discontinued hcq
One of the largest study
Methods: A retrospective chart review was performed on the medical records of patients diagnosed with SLE between July 1, 2006, and June 30, 2016.
Results -
509 patients continued hcq for mean -8years
172 patients discontinued hcq
Patients who received HCQ for less than 1 year before discontinuation (median duration of HCQ treatment was 2.5 months) were more likely to experience SLE flares compared with those who continued HCQ for more than 1 year (13.1% vs 5.7%, P = 0.019)
Efficacy of steriods in SLE -
https://pubmed.ncbi.nlm.nih.gov/17075807/
This study is prospective, randomized, double-blind, placebo-controlled trial, 154 patients were evaluated monthly for up to 18 months, with measurements of C3a, C3, C4, CH50, and anti-dsDNA levels.
Patients who remained clinically stable but showed serologic evidence of an SLE flare (elevation of both the anti-dsDNA level by 25% and the C3a level by 50% over the previous 1-2 monthly visits) were randomized to receive either prednisone or placebo therapy at a dosage of 30 mg/day for 2 weeks, 20 mg/day for 1 week, and 10 mg/day for 1 week.
41 patients included in study
21 randomised to Prednisone and 20 to placebo group
No flares in steriod group vs 6 flares in placebo group .
And the patients who received placebo required high dose of steroid +- immunosuppressive therapy .
Conclusion - short-term corticosteroid therapy may avert a severe flare.
Bisphosphonates -
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(88)92721-3/fulltext
In a prospective, randomised, placebo-controlled trial comparing the effect of (3-amino-1-hydroxypropylidene)-1,1-bisphosphonate (APD) (150 mg/day) plus calcium (1 g/day) with
that of calcium alone on the bone mass of patients receiving long-term glucocorticoid therapy,
the mean metacarpal cortical area in patients receiving APD increased by 1·2% between 0 and 6 months (p < 0·06) and then remained stable between 6 and 12 months.
In contrast, this index progressively declined in the placebo group (p <0·05 at 12 months). The two groups differed significantly in the changes at both 6 and 12 months (p<0·01).
Mean vertebral mineral density, as measured by quantitative computed tomography, increased by 19·6% over 12 months in the APD group (p<0·02) but showed a non-significant decline of 8·8% in controls. The differences between the changes were again significant (p<0·005).
The American College of Rheumatology recommendations for prevention of glucocorticoid-induced osteoporosis
Candidates for therapy:
Patients initiating glucocorticoids (prednisone equivalent of 5 mg/day or higher) with plans for treatment for more than three months
Patients taking long-term glucocorticoids (prednisone equivalent of 5 mg/day or higher)
Guidelines:
Modify lifestyle risk factors (avoiding smoking and excess alcohol, weight-bearing exercises).
Initiate Calcium (1000 to 1500 mg/day) and Vitamin D (800 IU/day) supplementation.
Prescribe bisphosphonates (use with caution in premenopausal women because of insufficient data on the potential for harm to the fetus in women who become pregnant while currently or recently receiving bisphosphonates).
Replace gonadal sex hormones if deficient.
Consider calcitonin as second-line agent if bisphosphonates are contraindicated or not tolerated.
In patients on long-term glucocorticoids (prednisone equivalent of 5 mg/day or higher), measure bone mineral density (BMD) at lumbar spine and/or hip at the initiation of glucocorticoid therapy. If T-score is below −1, then prescribe bisphosphonate or calcitonin. Repeat bone densitometry every year as long as glucocorticoid therapy continues.
What is the efficacy of using primary PPI prophylaxis during initiation of any corticosteroids to prevent Gi ulcers?
1991, a nested case-control study of 1415 patients found that ulcer risk was only increased in concurrent users of non-steroidal anti-inflammatory drugs (NSAIDs): RR 1.1 for corticosteroid alone, RR 4.4 for corticosteroid use in patients already on NSAIDs, RR 14.6 for corticosteroid and NSAIDs compared to controls .
d) Please share any reports around similar patients with SLE and TB meningitis?
https://pubmed.ncbi.nlm.nih.gov/10067053/
Here they discussed 51yr old female with SLE and developed tubercular meningitis with obstructive hydrocephalus after 14days of immune adsorption therapy .
She was started on ATT and patient was found to improve symptomatically.
Any reports of normal csf leukocyte count and normal csf protein in meningitis?
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-4204-z
This is systemic review of cases with normal CSF in meningitis.
A total of 124 cases from 51 articles were included. Causative organisms were primarily bacterial (99 cases). Outcome was reported in 86 cases, 27 of which died and 59 survived. Mortality in viral, fungal and bacterial organisms was 0, 56 and 31%, respectively.
Meningitis in the absence of pleocytosis on CSF is rare. If this occurs, causative organism is likely bacterial.
What could be the probable cause for a normal csf leukocyte count in a patient with chronic meningitis?
e) What is the sensitivity and specificity of ANA in the diagnosis of SLE?
https://pubmed.ncbi.nlm.nih.gov/8678710/
The estimated sensitivity and specificity of the ANA test for SLE were 100% and 86%, respectively. For other rheumatic diseases, sensitivity and specificity were 42% and 85%, respectively. The positive predictive value of the ANA test was 11% for SLE and 11% for other rheumatic diseases.
3-1)What was the research question in the above thesis presentation?
To study the association of serum magnesium levels in type 2 diabetes mellitus
2) What was the researcher's hypothesis?
Low Serum Magnesium levels is associated with development and progression of diabetic complications .
The deficiency of magnesium can lead to a variety of diseases, such as
impaired glucose tolerance
insulin resistance
abnormal lipid metabolism
Some studies have revealed that abnormal magnesium metabolism may lead to the occurrence and development of diabetes, diabetic microvascular and macroangiopathy complications
lower serum magnesium level can affect the development and progression of diabetic retinopathy and diabetic nephropathy.
3) What is the current available evidence for magnesium deficiency leading to poorer outcomes in patients with diabetes?
https://jfmpc.com/article.asp?issn=2249-4863;year=2019;volume=8;issue=5;spage=1671;epage=1677;aulast=Kumar
Study duration: The study was conducted over a period of 18 months from March 2014 to September 2015.
Study design: This was a cross-sectional observational study.Double blinded .
Group 1 (Case): T2DM with hypomagnesemia (S. Mg <1.7 mg/dL).
Group 2 (Control): T2DM with normal magnesium level (S. Mg 1.7–2.7 mg/dL).
The number of subjects in group 1 was 110, whereas in group 2, it was 140, in accordance with the sample size calculation.
What was the research question in the above thesis presentation?
Will salt restricted diet decrease BP
Does 24 hr urine sodium excretion reflect dietary intake .
What was the researcher's hypothesis?
Hypothesis is that, salt restriction doesn't effect blood pressure in all the individuals in the same way, and salt resistant individuals don't benefit from a restricted diet as much as a salt sensitive individual.
What is the current available evidence for the utility of monitoring salt excretion in the hypertensive population
The 24hr urinary sodium is a reflection of dietary sodium, and has better results than dietary recall method
http://repository-tnmgrmu.ac.in/6518/
https://www.tandfonline.com/doi/full/10.1080/07853890.2020.1780469
Aim - The objective was to evaluate whether sodium intake, assessed with the gold standard 24-h urinary collections, was related to long-term incidence of death, cardiovascular disease (CVD) and diabetes mellitus (DM).
Methods : A cohort of 4630 individuals aged 25–64 years collected 24-h urine samples in 1979–2002 and were followed up to 14 years for the incidence of any CVD, coronary heart disease (CHD), stroke, heart failure (HF) and DM event, and death.
Conclusion: During the follow-up, we observed 423 deaths
424 CVD events (288 CHD events, 142 strokes, 139 HF events) and 161 DM events. Compared with the highest quartile of salt intake, persons in the lowest quartile had a lower incidence of CVD (hazard ratio [HR] 0.70; 95% confidence interval [CI], 0.51–0.95, p = .02), CHD (HR 0.63 [95% CI 0.42–0.94], p = .02) and DM (HR 0.52 [95% CI 0.31–0.87], p = .01). The results were non-significant for mortality, HF, and stroke.
3) Please critically appraise the full text article linked below:
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2003.01233.x
Aspirin in the prevention of progressing stroke: a randomized controlled study.
Double blinded ,placebo controlled randomised trail.
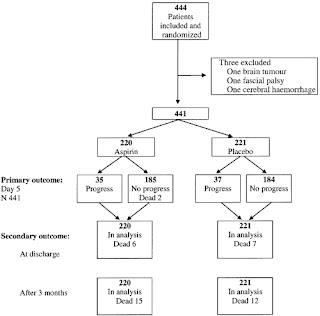
P-444 patients were included in the study,placebo -221 ,aspirin group - 220
Interventions. Aspirin (325 mg) or placebo was given once daily for five consecutive days.
C- Aspirin vs placebo .
Main outcome measures. Neurological assessments were carried out three times daily during the treatment period to detect progression of at least two points in the Scandinavian Stroke Supervision Scale. Patient outcome was followed up at discharge and at 3 months.
This study aimed at determining efficacy of Aspirin in preventing progression of new onset Ischemic stroke who were
not on antiplatelet drugs previously .
Drawback is it doesn't include - Patient with complete paresis .
It is a draw back of this study that it was so protracted. On the positive side and in spite of this, there have been a very limited number of persons involved and the main investigators have been able to take part in and supervise the work the whole time.
The main results of the trial showed that aspirin treatment did not significantly reduce the rate of stroke progression. The progression rate was 15.9% amongst patients treated with aspirin and 16.7% for those on placebo. In the aspirin group, the relative risk was 0.95 (95% CI 0.62–1.45).
They conclude that the present trial could not prove effects of the calculated size nor disprove smaller positive effects of aspirin in the prevention of stroke progression.
1. Did the study address a clearly focused
research question?- Yes
2. Was the assignment of participants to
interventions randomised?- yes
3. Were all participants who entered the study
accounted for at its conclusion?- No
4. • Were the participants ‘blind’ to
intervention they were given?- Yes
• Were the investigators ‘blind’ to the
intervention they were giving to
participants?-Yes
• Were the people assessing/analysing
outcome/s ‘blinded’?- No
5. Were the study groups similar at the start of
the randomised controlled trial?- Yes
6. Apart from the experimental intervention, did
each study group receive the same level of
care (that is, were they treated equally)?- Yes
7. Were the effects of intervention reported
comprehensively?-
•Was a power calculation undertaken?- Yes
• What outcomes were measured, and were
they clearly specified?-Neurological assessments were carried out three times daily during the treatment period to detect progression of at least two points in the Scandinavian Stroke Supervision Scale. Patient outcome was followed up at discharge and at 3 months.
• How were the results expressed? For
binary outcomes, were relative and
absolute effects reported?- Yes
• Were the results reported for each
outcome in each study group at each
follow-up interval?- Yes
• Was there any missing or incomplete data?- Cause of progression , underlying etiology,size of stroke .
• Was there differential drop-out between the
study groups that could affect the results?- No
• Were potential sources of bias identified?
• Which statistical tests were used? Statistical comparisons to test differences between the two groups were made by use of the Student's t‐test for uncorrelated means, after validation for normal distribution by use of the Shapiro–Wilke's test. The within‐group analysis was made by using parewise Student's t‐test for correlated means
• Were p values reported?Yes
8. Was the precision of the estimate of the
intervention or treatment effect reported?
CONSIDER:
• Were confidence intervals (CIs) reported?- Yes.
9. Do the benefits of the experimental
intervention outweigh the harms and costs?
CONSIDER:
• What was the size of the intervention or
treatment effect? - small size
• Were harms or unintended effects
reported for each study group?- yes
• Was a cost-effectiveness analysis
undertaken? (Cost-effectiveness analysis
allows a comparison to be made between
different interventions used in the care of
the same condition or problem.)- yes
10. Can the results be applied to your local
population/in your context?- Yes
11. Would the experimental intervention provide
greater value to the people in your care than
any of the existing interventions?- No
4) Please mention your individual learning experiences from this month.
I'm posted in cardiology for this month.
Below is the blog link to the cases I have seen and prepared online record .
https://draft.blogger.com/blog/posts/5008145020970757617
Jan 1-Reported in the department after finishing paper work
Jan 2- Attended rounds , managed icu patient,watched coronary angiogram and PTCA procedure .
Jan 4- Attended a patient with complete heart block ,who underwent Temporary pace maker insertion and later permanent pace maker .
Jan 5- presented patient with Valvular heart disease .
Jan 6- attended PG counseling program
Attended 2-4 pm session - thesis presentation .
Jan 7-Followed rounds ,examined patients .Learnt about thrombolytic therapy in MI
Jan 8- Patient had sudden cardiac arrest ,did CPR ,2d echo showed pericardial effusion - Patient had lv free wall rupture , electromechanical dissociation .
Read about free wall rupture and management options
https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-019-1063-x
Jan 9- took detailed history and examined 52/ M patient with chronic heart failure - Valvular heart disease .
Jan 11-Attended op from 9-5 pm , discussed cases with HOD sir ,learnt about murmurs ,TMT .
Performed 2d echo during rounds to measure improvement of LV contractility after PTCA and to look for lvedp.
Jan 12- Took history and examined 26/ F with MVP and repair done .
Now presented with stuck valve.
Read about stuck valve.
Jan 15-I was taught about TMT,indications for Mitral valvue replacement in MS and MR
Read about MS and MR from Harrison's principles of medicine .
Jan 16- Took detailed history ,examined her and performed 2d echo , prepared online blog of 42/ F with valvular heart disease.
Admitted 3 patients with Acute MI , managed them overnight
5)
https://vamsikrishna1996.blogspot.com/2021/01/36-year-male-presented-to-casualty-at.html?m=
a) What are the possible reasons for the 36 year old man's hypertension and CAD described in the link below since three years?
-Smoking
-alcohol
-HTN
- Atherosclerosis
- hyperlipidemia
b) Please describe the ECG changes and correlate them with the patient's current diagnosis.
Ecg changes -
Irregular rhythm ,normal axis .
Biphasic T waves in V1- V3 - wellens sign - suggestive of LAD occlusion- new changes.
VPC - unifocal ,arising from Right ventricle ,from apex to base .
With poor R wave progression ,QS complex from v1-v2.( old MI )
c) Share an RCT that provides evidence for the efficacy of primary PTCA in acute myocardial infarction over medical management. Describe the efficacy in a PICO format.
https://jamanetwork.com/journals/jama/fullarticle/194837
Objective To determine whether treatment of acute MI with primary PCI is superior to thrombolytic therapy at hospitals without on-site cardiac surgery and, if so, whether superiority is durable.
Design - The Atlantic Cardiovascular Patient Outcomes Research Team prospective- C-PORT trail , randomized trial conducted from July 1996 through December 1999.
Patients Four hundred fifty-one thrombolytic-eligible patients with acute MI of less than 12 hours' duration associated with ST-segment elevation on electrocardiogram.
Interventions After a formal primary PCI development program was completed at all sites, patients were randomly assigned to receive primary PCI (n = 225) or accelerated tissue plasminogen activator (bolus dose of 15 mg and an infusion of 0.75 mg/kg for 30 minutes followed by 0.5 mg/kg for 60 minutes; n = 226). After initiation of assigned treatment, all care was determined by treating physicians.
C- PCI vs thrombolysis
Main Outcome Measures Six-month composite incidence of death, recurrent MI, and stroke; median hospital length of stay.








Comments
Post a Comment