February exam
February exam
Below is the answer sheet for bimonthly exam of February .where in after going through the given patient related data and after reviewing the literature I quote few paragraphs from the articles I shared below .Few pictures are from Harrison’s textbook of medicine and few from online search articles .
50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
More here: https://archanareddy07.blogspot.com/2021/02/50m-with-parkinsonism.html?m=1
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Elderly male patient who was a chronic alcoholic and smoker ,aggressive personality came with complaints of
Frequent falls , running into the objects,self talking ,involving less in the conversations ,difficulty in keeping eyes open ,involuntary closure of eyelids since 1.5 years -slow but gradually progressive symptoms that brought him to the hospital . Taking all these into considerations and examination findings like decreased blink rate ,decreased arm swing,stooping posture ,postural instabilitity -PROGRESSIVE SUPRA NUCLEAR PALSY was our main diagnosis .
https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-019-0160-1
The constellation of parkinsonism and cognitive, speech, and oculomotor features in PSP reflect marked neuronal degeneration at different levels of the CNS, including the basal nucleus of Meynert, the pallidum, subthalamic nucleus, superior colliculi, mesencephalic tegmentum, substantia nigra (both pars compacta and reticulata), locus coeruleus, red nucleus, reticular formation, vestibular nuclei, cerebellum, and spinal cord.
As the interstitial nucleus of Cajal (INC) contributes to vertical gaze holding, inactivation of this structure causes a restricted range of vertical eye movement without inducing slow saccades
Problem representation and anatomical localization :
1-Running into the objects ,drooping of eyelids --EYELID OPENING APRAXIA —
Possible causes and anatomical localization include -
Muscles involved in opening eyelids
A-levator palpebrae superioris-LPS is supplied by occulomotor nerve
B-Mullers muscle
C-Frontalis muscle
cerebral cortex, basal ganglia, and superior colliculus (SC) are thought to play a role in disinhibition of leavator palpebra superioris
D-Orbicularis oculi -closes eyelids
E-Cerebral cortex -provides promotor control for eyelid movements,medial frontal lobes including supplementary area involved in control of blinking
F-Substabtia Nigra pars reticulata-dopamine depletion decreases blink rate -SEEN WITH PARKINSON PATIENT .
G-superior colliculus
EYELID DISORDERS - Droopy eyelids can be caused by neurogenic -innervational failure or LPS damage -myogenic Ptosis
Causes of neurogenic ptosis include :
;third cranial nerve palsy
• Horner syndrome
• Myasthenia gravies
• botulism
• Gullian Barre syndrome
• chronic inflammatory demyelinating polyneuropathy
MYOGENIC PTOSIS :
Congenital ptosis
Eyelid trauma /surgery
Mitochondrial myopathy
Oculi pharyngeal dystrophy
Myotonic dystrophy
Herpes zoster
Chronic topical steroid use
history of frequent falls :
Falls in elderly patient with background history of slowness and decreased expressiveness - would suggest autonomic instability or postural instability seen with parkinson patient .
Cause of falls : Ataxial rigidity
Bradykinesia
Loss of postural reflexes
Freezing
Visual vestibular component
B) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
The exact cause of psp is unknown .The hallmark of the disease is accumulation of protein tau in nerve cells in the brain -accumulation leads neuronal death .
Usually sporadic,very rare cases muatation in the gene MAPT is identified .
There are several theories about PSP's cause. A central hypothesis in many neurodegenerative diseases is that once the abnormal aggregates of proteins like tau form in a cell, they can affect a connected cell to also form the protein clumps. In this way the toxic protein aggregates spreads through the nervous system. How this process is triggered remains unknown. One possibility is that an unconventional infectious agent takes years or decades to start producing visible effects (as is seen in disorders like Creutzfeldt-Jakob Disease). Another possibility is that random genetic mutations, of the kind that occur in all of us all the time, happen to occur in particular cells or certain genes, in just the right combination to injure these cells. A third possibility is that there is exposure to some unknown chemical in the food, air, or water which slowly damages certain vulnerable areas of the brain.
Diagnostic approach to patient with atypical parkinsonism.
 |
| Red flag signs differentiating atypical Parkinsonism from PD |
 |
| Variants of psp |
Gait instability and early falls are key features of PSP and distinguish it from other parkinsonian syndromes
Complete gaze palsy and involuntary ocular fixation (as well as lack of eye blink) contribute to the classic “Mona Lisa” stare or stone face.
Rocket sign” occurs in patients with PSP who have lost insight into their postural instability and “rocket” out of their chair without assistance, resulting in a high risk for falling. Retropulsion and unchecked sitting (falling into their chair) are also common.
 |
| Overlap of Parkinsonian syndromes |
 |
| Overlap of neurodegenerative proteinopathies. |
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5567217/
C) What is the efficacy of each of the drugs listed in his current treatment plan.
Treatment :
1 . Tab. SYNDOPA 110mg PO TID
2. Tab. METFORMIN 500mg PO OD
There are variants of psp . Patients with psp + Parkinsonism predominant patients might improve initially with levodopa .
PSP-parkinsonism in particular is often levodopa responsive initially and contrasts with that observed in classic Richardson syndrome and other variants.
I have not found RCT comparing levodopa vs placebo in psp .
Metformin was given for management of diabetes
Metformin MOA -
Decreases hepatic gluconeogenesis
Increases peripheral uptake of glucose
Increases insulin sensitivity
2) Patient was apparently asymptomatic 2 years back then he developed weakness in the right upper and lower limb, loss of speech.
More here: https://ashfaqtaj098.blogspot.com/2021/02/60-year-old-male-patient-with-hrref.html?m=1
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
60 year old male patient who is a chronic alcoholic with history of CVA ,presented with progressive dyspnea since 2 months associated with pedal edema ,abdominal distension ,decreased urine output ..
Anatomical localization of current problem - SHORTNESS OF BREATH - progressed from grade 2 to grade 4 with orthopnea,PND —-left ventricular failure - it could be either due to
A) systolic heart failure
B)diastolic heart failure
What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Etiologies - coronary heart disease -ICMP
Cardiomyopathies -DCMP
Valvular heart disease - predominantly left side
With examination findings - apex down and out -left ventricular dilatation.
ECG- showing QS Complexes with poor R wave progression in chest leads .
Echo suggesting regional wall motion abnormalities
Most likely diagnosis could be heart failure secondary to coronary artery disease .
Approach to patient with SOB -
With no revelant history of smoking and also no wheeze,no seasonal variations -respiratory cause of sob has been ruled out .
Sequence of events :
2 years back weakness of right upper and lower limb with brocas aphasia
F/b
2 months history of SO,pedal edema
- What is the efficacy of each of the drugs listed in his current treatment plan
Tab. Lasix 40 mg bd
Tab. Benfomet plus od
Tab. Telma 40 mg od
Tab. Met xl 50mg od
Tab. Aldactone 25mg od
Salt restriction <2gm/day
Fluid restriction<1.5lit/day
Lasix ,fluid and salt restriction are supportive management to decrease preload on the heart .
Spirinolactone + Telmisartan + beta blockers are now recommended therapy for the patient’s with -chronic heart failure with reduced ejection fraction according to recent guidelines .
Most efficacious is ARNI + other combination .
Below I share a article regarding the above combination therapy - it’s a systemic review-https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.116.003529
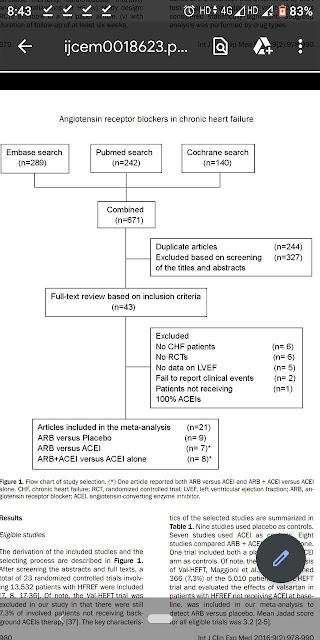
A systematic literature review identified 57 randomized controlled trials published between 1987 and 2015, which were compared in terms of study and patient characteristics, baseline risk, outcome definitions, and the observed treatment effects.
The random-effects network meta-analysis suggested that the combination of ACEI+BB+MRA was associated with a 56% reduction in mortality versus placebo (hazard ratio 0.44, 95% credible interval 0.26–0.66); ARNI+BB+MRA was associated with the greatest reduction in all-cause mortality versus placebo (hazard ratio 0.37, 95% credible interval 0.19–0.65).
Study Design
Phase II or III RCTs published in English.
P- Studies evaluating adults (aged ≥18 years) with chronic HFrEF (left ventricular ejection fraction <45%) and New York Heart Association class II–IV of varying etiology (ischemic and dilated cardiomyopathy) who were outpatients were included.
Interventions
All guideline-recommended drug classes: ACEIs, BBs, ARBs, and MRAs and an ARNI, administered alone or in combination (see Table I in the Data Supplement for eligible drug molecules).
Comparators
Placebo or any intervention of interest of a different class; comparisons within the same class were excluded (eg, ACEI versus ACEI).
Outcomes
Death because of any cause reported as an efficacy or safety end point.
ARB therapy was associated with a 14% reduc-
tion in cardiovascular mortality compared with
placebo without background ACEI treatment
(RR 0.86, 95% CI 0.74-0.99, I2=0%, P=0.010
- 52 year old male , shopkeeper by profession complains of SOB, cough ,decrease sleep and appetite since 10 days and developed severe hyponatremia soon after admission.
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Elderly male patient who is a diabetic and hypertensive came with symptoms of
Shortness of breath- grade 2-3 And Cough since 10 days .
With past history of similar complaints 1year back .
Possible differentials could be
- Acute coronary artery disease - Silent MI
- Community Acquired pneumonia .
- Acute on chronic heart failure
- Anemia
B)What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Approach to this patient :
We will screen for CAD - as patient falls under high risk for CAD
General -pallor +
Systemic examination - no obvious findings of pneumonia
ECG and echo showed no evidence of CAD ,
Concentric LVH with EF -62 percent .
X ray - bilateral pleural effusion with no consolidators changes .
Hemogram showed dimorphism anemia ( mostly due to Iron and vitB12 deficiency - Nutritional deficiency )
Etiology - Dimorphic anemia secondary to iron and vit B12 deficiency
Patient after admission suddenly developed hyponatremia .
Approach to hyponatremia
c) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient?
we shall discuss the role of vaptan treatment in chronic but not acute hyponatremia because the latter is rarely addressed in published literature.
THE INDICATIONS FOR VAPTANS ARE NOT CLEAR
1-First, we do not know how to distinguish between symptoms that are an indication for vaptan and those that are not.
2-Together, we lack information on which degree of severity of hyponatremia should give us reason to consider vaptan treatment.
3-Third, work by Gankam Kengne et al.28 suggested that patients with mild chronic hyponatremia fall to the ground more often than matched normonatremic controls .
We are unable to answer the question of whether elderly patients with chronic mild hyponatremia should be treated, for example, by a vaptan to correct hyponatremia and prevent fractures.
4-Fourth, in terms of indication for vaptan, the area least controversial might appear to be that of severe symptomatic (chronic) hyponatremia. A ‘hyponatremia-naive’ physician is likely to conclude that vaptans if anything should be promising in severe symptomatic hyponatremia. However, there are literally no published data on this. Clinical trials of vaptans have consistently excluded severe symptomatic hyponatremia from study because of ethical concerns (risk of worsening of severe symptoms when receiving placebo)
recent expert panel suggested that in severe symptomatic (chronic) hyponatremia, infusions of hypertonic saline should have priority over vaptan.30 This is an area of significant uncertainty. It has been pointed out that 3% NaCl may correct hyponatremia too quickly,31 or it may occasionally lead to pulmonary edema in SIAD(H). On the other hand, we have personal experience (PAG) that SIAD(H)-related severe symptomatic hyponatremia is a rewarding indication for vaptan. Thus, in the absence of a trial comparing fluid restriction plus 3% saline with vaptans in severe symptomatic hyponatremia, we do not have a database to make specific recommendations for or against vaptans.
Tolvaptan, a Selective Oral Vasopressin V2-Receptor Antagonist, for Hyponatremia | NEJM
SALT 1 ,SALT 2 Trails :
Hyponatremia (serum sodium concentration, <135 mmol per liter) is a predictor of death among patients with chronic heart failure and cirrhosis
In two multicenter, randomized, double-blind, placebo-controlled trials, the efficacy of tolvaptan was evaluated in patients with euvolemic or hypervolemic hyponatremia. Patients were randomly assigned to oral placebo (223 patients) or oral tolvaptan (225) at a dose of 15 mg daily
Inclusion : Patients had chronic heart failure, cirrhosis, or the syndrome of inappropriate antidiuretic hormone secretion (SIADH) in association with the hyponatremia.
Exclusion :Persons with psychogenic polydipsia, head trauma, postoperative conditions, uncontrolled hypothyroidism or adrenal insufficiency, or any hyponatremic condition associated with the use of medications that could have been safely withdrawn were ineligible.
Other exclusion criteria were recent cardiac surgery, myocardial infarction, sustained ventricular tachycardia or fibrillation, severe angina, cerebrovascular accident, or multiple strokes; systolic blood pressure of less than 90 mm Hg, central venous pressure of less than 5 cm of water, pulmonary-capillary wedge pressure of less than 5 mm Hg, a serum creatinine concentration of more than 3.5 mg per deciliter (309 μmol per liter), a Child–Pugh score of more than 10 (unless approved by the study's medical monitor), or a serum sodium concentration less than 120 mmol per liter in association with neurologic impairment; and the presence of severe pulmonary hypertension, urinary tract obstruction, uncontrolled diabetes mellitus, or progressive or episodic neurologic disease.
The present study was conducted primarily in the outpatient setting, without mandated fluid restriction or a change in the patient's medication regimen, such as use of diuretics, to treat the patient's primary disease. Tolvaptan was superior to placebo with respect to several measures, including the change in the average daily AUC for serum sodium concentrations from baseline to day 4 and from baseline to day 30, the mean serum sodium concentration at each visit, the time to normalized serum sodium concentrations, the percentage of patients with serum sodium concentrations that were normal on day 4 and on day 30, and the categorical change in the serum sodium concentration from baseline to day 4 and from baseline to day 30. Tolvaptan was superior to placebo from the first observation point (8 hours) after administration of the first dose until the last treatment day (day 30) in patients with either mild or marked hyponatremia and among patients with hyponatremia from all major causes. During the 7-day follow-up period, serum sodium concentrations reverted to degrees of hyponatremia that were equivalent to those associated with the use of placebo, indicating that the aquaretic effect of tolvaptan (excretion of electrolyte-free water) was required to maintain normal sodium concentrations in patients with chronic hyponatremia.
 |
| Study method |
 |
| Change in the Average Daily Area under the Curve (AUC) for the Serum Sodium Concentration from Baseline to Day 4 (Panel A) and from Baseline to Day 30 (Panel B). |
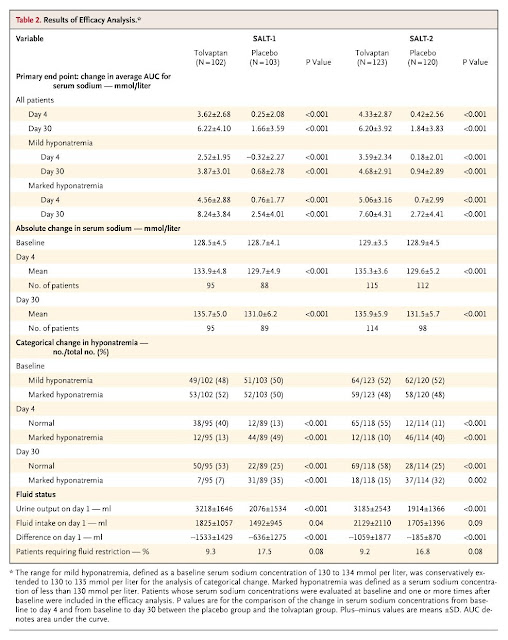 |
| Results of Efficacy Analysis. |
4) Please mention your individual learning experiences from this month.
I Have been posted in neurology - Seen opd along with sir and have learnt few topics
- traumatic brain injury
- Approach to headache
- Seizure disorder
- Dopa sensitivite dystonias
Learning points from central meets
1- Pulmonary alveolar microlithiasis
Presentation,x ray findings ,current therapy .
Role of genetics .
Lung transplant is the only treatment option available
2-acute abdomen in pregnancy - the possible medical and surgical causes and their management in brief
3-Euglycemic insulin therapy in calcium and beta blocker toxicity
Insulin act as positive ionotropic agent in patients with refractory hypotension in these toxicities .
It is now recommended as first line agent .
4-ARNEP effect - sudden increase in myocardial contractility with increase in after load .
ASHMANN phenomenon
Ashman phenomenon: a physiological aberration
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3669876/
The Fisch criteria for the diagnosis of Ashman phenomenon includes—a relatively long cycle immediately preceding the cycle terminated by the aberrant QRS complex, right bundle branch block (RBBB)-form aberrancy with normal orientation of the initial QRS vector, irregular coupling of aberrant QRS complexes and lack of a fully compensatory pause.2 The pathophysiology1 2 of Ashman phenomenon depends on the variability of relative refractory period of the conduction tissues depending upon the heart rate.
Learnt about Modified rapid sequence intubation in hypotension patients .
https://litfl.com/intubation-hypotension-and-shock/
A modified rapid sequence intubation (RSI) approach is usually preferred in shocked patients, including:
use of low dose, titrated induction agents to avoid haemodynamic compromise
avoidance of apnoea (e.g. via spontaneous breathing or supported ventilation) to avoid exacerbation of coexistent acidaemia
appropriate use of IV fluids and/or inotropes/ vasopressors
The mantra is “Resuscitate before you intubate!”
















Comments
Post a Comment